DAY RATE ATTENDANCE RECORD
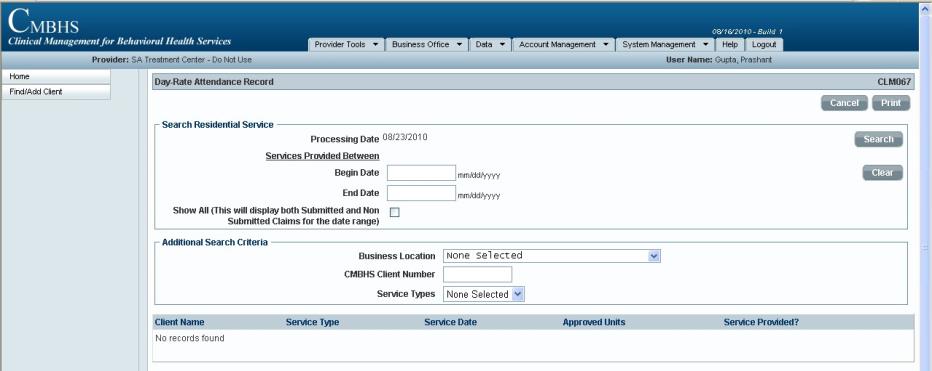
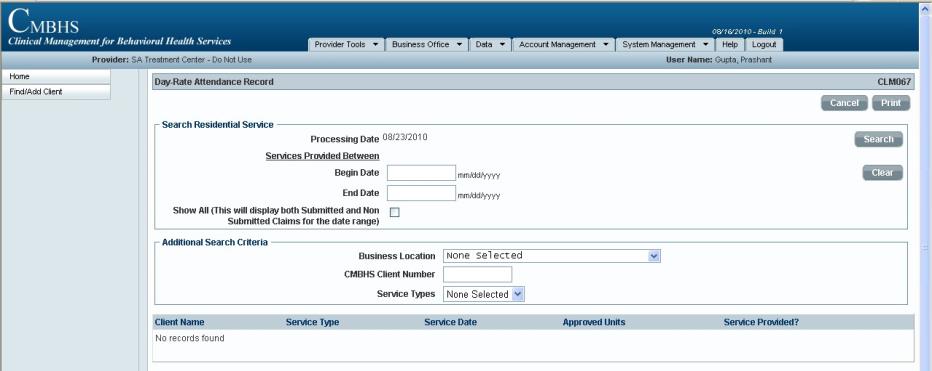
This function in Clinical Management for Behavioral Health Services (CMBHS) provides the user the place to document a client’s presence and participation in a Residential Service or other service that are billed on a day-rate basis and generate a claim for the service. These claims are also called Institutional Claims. Day rate attendance is documented on page CLM067.
CMBHS will generate a Day Rate Attendance Record for each day a client is receiving services based on the Service Begin and Service End documentation.
Before You Start
| SPECIAL INSTRUCTIONS FOR NorthSTAR SERVICE PROVIDERS: |
|
|
Business Rules for the Day Rate Attendance Record
- When the client has a Begin Service created for a service that requires use of a Day Rate Attendance Record, a Day Rate Attendance Record is created for the client.
- The Day Rate Attendance Record can be accessed by going to the client’s Client Workspace, and scrolling down toward the bottom of the page to the Document List.
- If you use the Day Rate Attendance Record to document a client’s attendance and participation in a service for billing purposes, you can and in some cases, you must, also create a progress note for a specific client. The progress note should automatically display as non-billable
How to Document Attendance on a Day Rate Attendance Record
How to Search for a Day Rate Attendance Record
How to Submit a Day Rate Attendance Record
- The submitted Day Rate Attendance record will create a claim which can now be viewed on the “Pending Claims” page under the Business Office menu on the Administrative toolbar at the top of your screen.
- When the “Pending Claims” menu item is selected, the Search Pending Claims page will display.
- Current"Pending Claims" can be located by using any combination of the data fields available on the Search Pending claims page. After filling in the search criteria,CLICK ON the “Search” button. Any pending claims during the time period.
- Review each pending claim for accuracy. Also, if the bottom left of the screen shows multiple pages, you must review each page before CLICKING ON the “Submit Claims” button.
- Select the appropriate Contract from the dropdown list in the Contract field and the system will check mark the “Submit Claims” box indicating that the claim(s) will be submitted for payment.
- Remember, if the “Financial Eligibility Number (FE#)" Column is blank, the client does not have a valid Financial Eligibility and the claim will not submit for payment.
- You will get a confirmation message that the claim was successfully submitted.
- CAUTION: If the “Financial Eligibility Number (FE#)" Column is blank, the client does not have a valid Financial Eligibility in his/her CMBHS record and the claim can not be submitted for payment.
- NOTE: Also, if the bottom left hand-side of the list, you see blue numbers such as 1, 2, 3, 4, 5, … this indicates that there are multiple pages, you must review each page beforeCLICKING ON the “Submit Claims” button.
NEXT,
CLICK HERE to go to 'MULTI-CLIENTS NOTES'